-
Leaky Gut Syndrome, or Intestinal Permeability, is a serious but often overlooked condition affecting an estimated 65% of the population. It occurs when the intestinal barrier becomes damaged, allowing harmful substances such as toxins, undigested food particles, and bacteria to leak into the bloodstream. This can trigger inflammation, disrupt immune function, and contribute to chronic health conditions.
Research has linked Leaky Gut Syndrome to autoimmune diseases,[1] neurological disorders,[2] digestive conditions, [3] and even mental health issues. Despite its widespread impact, many people remain unaware of its role in their health struggles.
The good news? Leaky Gut is reversible. By addressing the root causes, reducing inflammation, and repairing the intestinal lining, you can restore gut health and improve overall well-being.
What is Leaky Gut Syndrome?
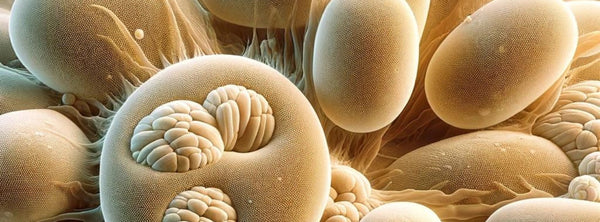
The digestive system is designed to absorb nutrients while keeping harmful substances out of the bloodstream. This is controlled by the intestinal barrier, which is made up of tight junctions between cells in the gut lining.
In a healthy gut, these junctions act like a security gate, allowing only properly digested nutrients to pass through. However, when the gut lining becomes damaged, these junctions loosen, creating microscopic gaps in the intestinal wall. As a result, toxins, bacteria, and undigested food particles can enter the bloodstream, triggering an immune response and widespread inflammation.
The result? Systemic health problems that go far beyond digestion.
Click on the tabs above for more information
-
Causes of Leaky Gut Syndrome
Leaky Gut Syndrome develops when the intestinal barrier is weakened due to chronic damage and inflammation. While this barrier is designed to protect the body by allowing nutrients in and keeping harmful substances out, certain dietary, lifestyle, and environmental factors can disrupt this balance. When this happens, toxins and harmful bacteria enter the bloodstream, fueling inflammation and immune dysfunction.
Below are some of the main contributors to Leaky Gut Syndrome and how they can negatively impact gut health.
Poor Diet
What you eat directly impacts gut health. The Standard Western Diet, high in processed foods, refined sugars, and unhealthy fats, damages the gut lining and disrupts gut bacteria balance. Some of the biggest dietary culprits include:
- Gluten & food allergens – Gluten, dairy, soy, and other common allergens can trigger immune responses and increase inflammation in the intestinal lining. In some people, gluten can activate zonulin, a protein that loosens tight junctions between gut cells, leading to increased permeability. Chronic exposure to inflammatory foods can damage intestinal cells and contribute to Leaky Gut.
- Refined sugars & processed foods – Feed harmful bacteria and yeast, worsening dysbiosis and disrupting the gut barrier. High sugar intake also increases inflammation, which can further weaken the gut lining.
- Excessive alcohol & caffeine – Irritate the gut lining and can increase intestinal permeability, especially when consumed in excess. Alcohol also depletes beneficial gut bacteria, further worsening dysbiosis.
- Low-fibre diets – Fibre is essential for feeding beneficial gut bacteria, which produce short-chain fatty acids (SCFAs) like butyrate that help strengthen the intestinal lining and regulate inflammation. Low fibre intake reduces mucus production, which acts as a protective layer over the gut lining. Without adequate mucus, the gut lining becomes more vulnerable to damage and permeability.
Medications That Damage the Gut
Certain medications, while sometimes necessary, can weaken the gut lining, disrupt gut bacteria, and increase inflammation. Frequent or long-term use of these drugs can compromise intestinal integrity and contribute to Leaky Gut Syndrome.
- Antibiotics – Used for treating bacterial infections, antibiotics do not distinguish between harmful and beneficial bacteria, leading to an imbalance in the gut microbiome (dysbiosis). [4] Some antibiotics have also been shown to increase intestinal permeability by directly affecting tight junctions in the gut lining. When beneficial bacteria are wiped out, harmful microbes can overgrow, further damaging the gut. [5]
- NSAIDs e.g., ibuprofen, aspirin, naproxen) – These drugs erode the protective mucus lining of the intestines, exposing the gut lining to irritation and inflammation. Over time, NSAIDs can cause microscopic tears in the gut wall, making it more permeable and increasing the risk of gut-related inflammation and disorders.
- Corticosteroids (e.g., prednisone, hydrocortisone) – While effective at reducing inflammation, corticosteroids thin the gut lining, making it more vulnerable to damage. They also alter gut bacteria composition, further increasing the risk of dysbiosis.
- Methotrexate – A commonly used immunosuppressive and chemotherapy drug, methotrexate can damage the intestinal lining, leading to increased gut permeability. [6] It alters gut bacteria composition (dysbiosis), reduces mucus production, and triggers inflammation, making the gut barrier more vulnerable to damage. Studies have linked methotrexate use to intestinal toxicity, microbiome imbalance, and increased risk of Leaky Gut Syndrome.
- Birth control pills & hormone replacement therapy (HRT) – Long-term use of synthetic hormones can disrupt the balance of gut bacteria, weaken the gut lining, and contribute to hormone-driven inflammation. Some studies suggest that oestrogen-based medications may increase gut permeability, exacerbating inflammatory conditions.
- Testosterone replacement therapy (TRT) – While beneficial for some, TRT can increase inflammatory markers in the gut and potentially contribute to gut lining dysfunction if not properly monitored.
- Chemotherapy & radiation therapy – These treatments directly damage intestinal cells, impairing the gut’s ability to regenerate and repair itself. Chemotherapy, in particular, is known to cause significant inflammation and permeability issues, leading to nausea, diarrhoea, and long-term gut dysfunction.
- Proton Pump Inhibitors (PPIs) & antacids – These medications reduce stomach acid, which is essential for proper digestion and protecting against harmful bacteria. Low stomach acid allows undigested food particles and pathogens to enter the intestines, triggering inflammation and contributing to gut imbalances.
Dysbiosis (Imbalance of Gut Bacteria)
A healthy gut microbiome is essential for digestion, immune function, and maintaining a strong intestinal barrier. It consists of trillions of beneficial bacteria that support gut integrity and keep harmful microbes in check. However, when this balance is disrupted, harmful bacteria, yeast, or parasites can overgrow, releasing toxins that inflame and weaken the gut lining—a condition known as dysbiosis.
Dysbiosis can increase intestinal permeability, making the gut more susceptible to Leaky Gut Syndrome. Some of the most common causes include:
- Poor diet – Diets low in fibre and high in sugar, processed foods, and unhealthy fats promote the overgrowth of harmful bacteria and yeast. Fibre feeds beneficial gut bacteria, while excess sugar and processed foods fuel pathogenic bacteria and Candida overgrowth, increasing inflammation and damaging the gut lining.
- Frequent antibiotic use – Antibiotics wipe out both harmful and beneficial bacteria, disrupting the gut’s delicate ecosystem. This imbalance can allow opportunistic bacteria and yeast to overgrow, compromising gut health and increasing intestinal permeability.
- Chronic stress – Stress alters gut function by reducing beneficial bacteria, impairing digestion, and increasing inflammation. Elevated cortisol levels can also weaken the gut lining, making it more susceptible to damage from harmful microbes.
- Bacterial, viral, or parasitic infections – Pathogenic infections release toxins that inflame and weaken the gut barrier. Conditions like SIBO (Small Intestinal Bacterial Overgrowth), Candida overgrowth, and parasitic infections can contribute to chronic gut inflammation and permeability.
Restoring balance in the gut microbiome is essential for healing the gut lining, reducing inflammation, and preventing further damage.
Chronic Stress
Stress isn’t just a mental or emotional burden—it has a direct and measurable impact on gut health. When stress becomes chronic, it disrupts digestion, weakens the gut lining, and contributes to inflammation, making it a significant factor in Leaky Gut Syndrome.
How stress damages the gut:
- Increases cortisol levels – Chronic stress triggers the release of cortisol, a hormone that, in excess, weakens the gut lining and increases intestinal permeability.
- Reduces digestive function – Stress diverts blood flow away from the digestive system, leading to reduced stomach acid and enzyme production. This results in poor digestion, increased gut irritation, and a higher likelihood of undigested food particles triggering immune responses.
- Disrupts gut bacteria balance – Stress alters the gut microbiome by reducing beneficial bacteria and promoting the growth of harmful microbes, contributing to dysbiosis and further weakening the intestinal barrier.
- Increases inflammation – Prolonged stress triggers inflammatory responses throughout the body, including in the gut, worsening intestinal permeability and making the gut lining more vulnerable to damage.
Chronic stress has been linked to conditions like IBS, anxiety, autoimmune diseases, and widespread inflammation. Managing stress through lifestyle changes, relaxation techniques, and quality sleep is an important step in healing Leaky Gut.
Chemical & Environmental Toxin Exposure
Every day, we are exposed to chemicals, heavy metals, and environmental toxins that can disrupt gut health and contribute to Leaky Gut Syndrome. These toxins can weaken the gut lining, trigger inflammation, and alter the gut microbiome, making the intestines more vulnerable to damage.
Common sources of toxins that impact gut health:
- Pesticides and herbicides – Chemicals like glyphosate, commonly found in non-organic produce, have been shown to disrupt gut bacteria and increase intestinal permeability. They can also interfere with digestive enzymes, making it harder for the body to break down food properly.
- Food additives and preservatives – Artificial sweeteners, emulsifiers, and processed food chemicals can irritate the gut lining, promote dysbiosis, and contribute to inflammation. Some additives, like carrageenan and certain food dyes, have been linked to increased gut permeability.
- Heavy metals – Mercury, lead, arsenic, and aluminium, often found in contaminated water, seafood, dental fillings, and some medications, can accumulate in the body and damage the gut lining. Heavy metal exposure is also associated with increased oxidative stress, which contributes to chronic inflammation in the intestines.
- Household chemicals and pollutants – Air pollution, cleaning products, plastics (such as BPA and phthalates), and synthetic fragrances contain toxins that can disrupt hormone balance and negatively impact gut bacteria. Long-term exposure to these chemicals has been linked to immune dysfunction and increased gut permeability.
Click on the tabs above for more information
-
Health Conditions Linked to Leaky Gut
Leaky Gut Syndrome doesn’t just affect digestion—it can have far-reaching effects on the entire body. A compromised gut barrier allows toxins, bacteria, and undigested food particles to enter the bloodstream, triggering chronic inflammation and immune system dysfunction. Over time, this persistent immune activation can contribute to the development of various chronic health conditions.
Research has linked Leaky Gut to a wide range of issues, from digestive disorders and autoimmune diseases to neurological conditions and metabolic dysfunction. Below are some of the most common health conditions associated with intestinal permeability.
Digestive Disorders
Since Leaky Gut directly affects the intestines, digestive issues are among the most common consequences.
- Irritable Bowel Syndrome (IBS) – Leaky Gut can contribute to IBS by causing chronic inflammation, disrupting gut bacteria, and increasing sensitivity to certain foods. This can result in bloating, cramping, diarrhoea, constipation, and irregular bowel habits.
- Inflammatory Bowel Disease (Crohn’s, Ulcerative Colitis) – Leaky Gut plays a significant role in autoimmune gut disorders, where an overactive immune response causes chronic inflammation and damage to the intestinal lining.
- Food intolerances and allergies – When the gut barrier is weakened, undigested food particles leak into the bloodstream and trigger immune reactions. Over time, this can lead to the development of food intolerances, sensitivities, and increased allergic responses.
Autoimmune & Inflammatory Conditions
Leaky Gut has been identified as a key factor in autoimmune disease development. When foreign substances leak into the bloodstream, the immune system may mistake its own tissues for invaders, leading to chronic inflammation and autoimmunity.
- Rheumatoid arthritis – Leaky Gut has been linked to increased inflammation in the joints, triggering pain and stiffness characteristic of rheumatoid arthritis.
- Hashimoto’s thyroiditis – Studies show that increased intestinal permeability is common in thyroid disorders. Toxins and inflammatory molecules from the gut can contribute to immune system dysfunction, leading to attacks on the thyroid gland.
- Multiple Sclerosis (MS) – Leaky Gut can contribute to MS by increasing systemic inflammation, weakening the blood-brain barrier, and triggering immune dysfunction, which can worsen neuroinflammation and disease progression.
- Psoriasis, eczema, and other skin disorders – The gut and skin are closely connected, often referred to as the "gut-skin axis." When the gut barrier is compromised, toxins can be eliminated through the skin, leading to chronic inflammation, breakouts, rashes, and skin disorders like eczema, psoriasis, and rosacea.
Neurological & Mental Health Disorders
The gut-brain connection means that gut inflammation can significantly impact brain function, mood, and mental health.
- Anxiety and depression – Over 90% of serotonin, the "feel-good" neurotransmitter, is produced in the gut. When gut bacteria are imbalanced and inflammation is high, serotonin production is reduced, contributing to mood disorders.
- Brain fog and memory loss – Increased gut permeability can weaken the blood-brain barrier, allowing inflammatory compounds to enter the brain, leading to cognitive issues, lack of focus, and memory problems.
- ADHD and Autism Spectrum Disorders – Research has shown that individuals with ADHD and autism often have gut imbalances and increased intestinal permeability. The inflammation from a leaky gut may contribute to neurotransmitter imbalances and nervous system dysfunction.
Metabolic & Other Health Problems
Leaky Gut also affects metabolism, energy levels, and immune function, contributing to a wide range of chronic conditions.
- Chronic fatigue syndrome – Increased inflammation, poor nutrient absorption, and immune dysfunction caused by Leaky Gut can leave the body in a constant state of exhaustion.
- Insulin resistance and weight gain – Inflammation from Leaky Gut can disrupt metabolism and insulin signalling, leading to blood sugar imbalances, increased fat storage, and difficulty losing weight.
- Frequent infections – Since over 70% of the immune system is located in the gut, chronic gut inflammation can weaken the body’s ability to fight infections, leading to recurrent colds, flu, and other illnesses.
How Leaky Gut Affects Other Barriers in the Body
The intestinal barrier doesn’t function in isolation—it is closely connected to other protective barriers in the body, including the blood-brain barrier, skin barrier, lung barrier, and liver-gallbladder barrier. When the gut lining becomes compromised, inflammation and toxins can spread beyond the digestive system, affecting multiple areas of health.
The gut-brain connection – The blood-brain barrier is a protective layer that prevents harmful substances from entering the brain. When the gut becomes leaky, inflammatory molecules and toxins can enter the bloodstream and weaken the blood-brain barrier, making it more permeable. This has been linked to neurological disorders, mood imbalances, brain fog, memory loss, and cognitive decline. Studies suggest that conditions like anxiety, depression, Alzheimer’s disease, and even migraines may be worsened by chronic gut inflammation.
The gut-skin connection – The skin barrier is another critical defence system, and its health is directly influenced by the gut. When the gut is inflamed and unable to properly eliminate toxins, the body may push them out through the skin instead. This can lead to acne, eczema, psoriasis, rosacea, and other chronic skin conditions. Many people with these conditions see significant improvement when gut health is restored.
The gut-lung connection – Research has also linked Leaky Gut to lung health. The gut and lungs communicate through the gut-lung axis, and inflammation in the gut can contribute to asthma, allergies, and respiratory issues. A damaged gut lining may lead to an overactive immune response, increasing the risk of inflammatory lung conditions.
The Gut-Liver-Gallbladder Connection - The liver and gallbladder rely on a healthy gut to filter toxins and regulate digestion. When the gut becomes leaky, toxins, bacteria, and inflammatory molecules travel to the liver via the portal vein, overloading detox pathways and contributing to fatty liver disease, bile acid imbalances, and gallbladder dysfunction. A weakened gut barrier can also disrupt bile flow, increasing the risk of gallstones, sluggish digestion, and liver inflammation.
Since these protective barriers are interconnected, healing the gut is a key step in improving brain function, skin health, liver detoxification, and overall immunity.
Click on the tabs above for more information
-
How to Heal Leaky Gut
Healing Leaky Gut requires a comprehensive, step-by-step approach to repair the intestinal lining, rebalance gut bacteria, and reduce inflammation. Without proper intervention, a compromised gut barrier can continue to fuel chronic health issues, autoimmune conditions, and systemic inflammation. By restoring gut integrity, we not only improve digestion but also support brain function, skin health, immune resilience, and overall well-being.
Since everyone’s gut health is different, the healing process varies depending on the severity of symptoms. Typically, gut healing follows a two-phase approach:
- Addressing dysbiosis (2-4 weeks) – Eliminating harmful bacteria, yeast, and parasites that contribute to gut dysfunction.
- Repairing and strengthening the gut lining (4-12 weeks) – Supporting digestion, reducing inflammation, and rebuilding the intestinal barrier.
Once healing is complete, ongoing gut maintenance helps prevent future issues and supports long-term digestive health.
Testing for Leaky Gut
Several tests can help assess the integrity of the gut lining and confirm Leaky Gut Syndrome:
- Lactulose/Mannitol Test – Measures intestinal permeability by tracking how much of these sugars pass through the gut lining into the bloodstream.
- Zonulin Test – Zonulin is a protein that regulates tight junctions in the gut. Elevated zonulin levels indicate increased intestinal permeability and a weakened gut barrier.
While testing can provide useful insights, symptoms alone—such as bloating, food sensitivities, fatigue, and chronic inflammation—are often enough to suggest Leaky Gut and warrant targeted treatment.
Step 1: Restore Gut Bacteria (Address Dysbiosis)
A balanced gut microbiome is essential for healing. If dysbiosis (bacterial imbalance) is present, it must be corrected first before repairing the gut lining. This phase typically lasts 2-4 weeks, depending on symptoms like bloating and gas.
The following supplements help eliminate harmful microbes and restore beneficial bacteria:
- Intestinal Cleanse – Supports the removal of harmful bacteria, parasites, and toxins that contribute to gut inflammation.
- Multibac 10 – A multi-strain probiotic that replenishes beneficial bacteria and restores microbial balance.
- SacchroBiotic – A probiotic yeast that helps crowd out harmful microbes and supports immune function.
Step 2: Improve Digestion & Repair the Intestinal Lining
Once dysbiosis has been addressed, the repair phase begins, typically lasting 4-12 weeks, depending on the severity of Leaky Gut. This stage focuses on improving digestion, reducing inflammation, and rebuilding the gut lining.
To support digestion and nutrient absorption:
-
Digestive Support – Stimulates digestive qi, stomach acid, bile, and enzyme production to enhance digestion and reduce gut irritation.
To repair and soothe the intestinal lining:
- Intestinal Repair – A blend of L-Glutamine, Slippery Elm, Aloe Vera, and Marshmallow Root to reduce inflammation, protect gut cells, and rebuild the intestinal barrier.
- Revitalise – Provides essential prebiotic fibres to feed beneficial gut bacteria, support microbiome balance, and enhance digestion.
- Multibac 10 – A high-potency probiotic to restore microbial diversity and reinforce gut barrier integrity.
These supplements work together to strengthen the gut lining, enhance nutrient absorption, and promote overall digestive health.
Step 3: Maintain Gut Health Long-Term
After healing the gut, ongoing maintenance is crucial to prevent future gut issues. A fibre-rich diet and targeted supplementation help sustain gut health and prevent dysbiosis from returning.
- Intestinal Maintain – A blend of seven different fibre types (soluble, insoluble, and prebiotic) combined with slippery elm, marshmallow root, and yucca to support gut barrier integrity and overall digestion.
Additionally, making lifestyle changes such as reducing stress, eating a whole-food diet, staying hydrated, and prioritising sleep will help maintain a strong gut lining and prevent future relapses.
Comprehensive Gut-Healing Support
For a structured and effective approach, we offer a Leaky Gut Support Pack, which includes all the essential supplements needed for repair, along with dietary recommendations and a treatment guide.
Healing Leaky Gut is a journey, but with the right approach, gut function can be fully restored, leading to better digestion, reduced inflammation, and improved overall health.
Take the Next Step Toward Gut Healing
Leaky Gut Syndrome is a major contributor to chronic health issues, but it can be healed. By addressing the root causes, restoring gut balance, and repairing the intestinal lining, you can regain control of your digestion, immunity, and overall well-being.
If you're experiencing digestive discomfort, food sensitivities, mental health issues or inflammation and need expert guidance, we’re here to help.
👉 Book an appointment with us today to get a personalised plan for healing your gut.
Know someone who could benefit from this? Share this article with them!
Disclaimer:
This information is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Please consult a healthcare professional before starting any new health protocol.